What Is Snoring?
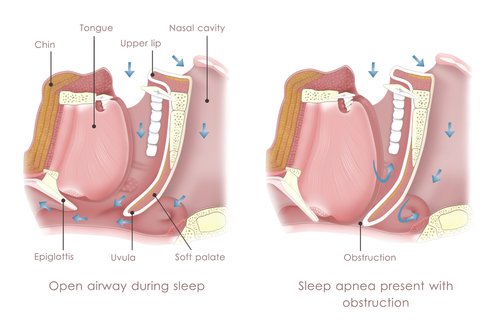
Snoring is the noisy breathing that occurs during sleep, characterised by a rattling, snorting, or grumbling sound. It happens when air flows past relaxed tissues in the throat, causing them to vibrate.
While occasional snoring is usually harmless, chronic or loud snoring may signal an underlying condition such as obstructive sleep apnea.
What Causes Snoring?
Snoring occurs when the muscles in the soft palate, tongue, and throat relax during sleep, causing tissues to partially block airflow and vibrate. The narrower the airway, the more forceful the airflow, resulting in louder snoring.
Several factors can contribute to this obstruction and vibration:
- Anatomy – A low, thick soft palate, extra throat tissue (often due to being overweight), or an elongated uvula can all narrow the airway.
- Nasal Problems – Chronic congestion, allergies, colds, or structural issues like a deviated septum or polyps can block airflow through the nose.
- Alcohol and Sedatives – These can overly relax the throat muscles, restricting airflow through the nose and throat.
- Sleep Position – Snoring is often louder when sleeping on the back, as gravity can further narrow the airway.
- Sleep Deprivation – Not getting enough rest can lead to deeper muscle relaxation, increasing the chance of snoring.
- Weight – Excess weight, especially around the neck, can compress the airway.
- Family History – Genetic factors can influence airway structure and muscle tone, making snoring more likely.
What Is Obstructive Sleep Apnea (OSA)?
Obstructive Sleep Apnea (OSA) is a form of breathing disorder that occurs during sleep.
Patients with OSA have difficulty breathing when they sleep because their upper air passages in the nose and
throat collapse and obstruct more easily than those who do not have OSA. This may occur due to nasal blockage,
enlarged tonsils, a large tongue (in relation to the mouth) or a small-sized jaw.
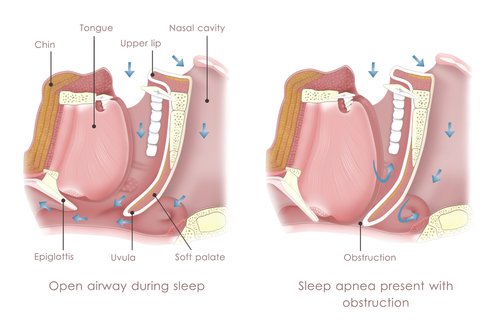
During these obstructive episodes, the patient is trying to breathe but is unable to because of the obstruction.
He may stop breathing partially (hypopnea) or completely (apnea).
During such episodes, the oxygen concentration in the body drops. As a result, the patient's oxygen level in the
body decreases. This causes great stress on the heart because it now has to pump harder and faster to supply
oxygenated blood to the rest of the body.
If left untreated, this can lead to serious and long-term health consequences as the heart and brain’s blood
supply could easily be compromised.
When Does Obstructive Sleep Apnea Occur?
Upper airway obstruction from OSA may occur anytime during sleep.
They, however, occur more often during deep sleep (S3) and dream sleep (REM) because the muscles are more relaxed
during these sleep periods.
The patient is trying hard to breathe but is unable to get air into the lungs because of upper airway collapse.
- Middle-aged males
- Overweight individuals
- Patients with certain hormone problems (e.g. hypothyroidism)
- Patients with enlarged tonsils (e.g. from frequent sore throats)
How Is Obstructive Sleep Apnea Diagnosed?
The only way to diagnose OSA accurately is to do an overnight sleep study, which can be done either at home or in
the hospital.
Even if screening questionnaires, the patient’s medical history, and physical examination all suggest that the
patient may have OSA, it is ultimately still not the most reliable, and the decision to treat is always based on
the sleep study result.
(A sleep study provides information on the number of apneic and hypopneic episodes each night and their effect on
the cardiorespiratory system.)
Common Sites of Obstruction
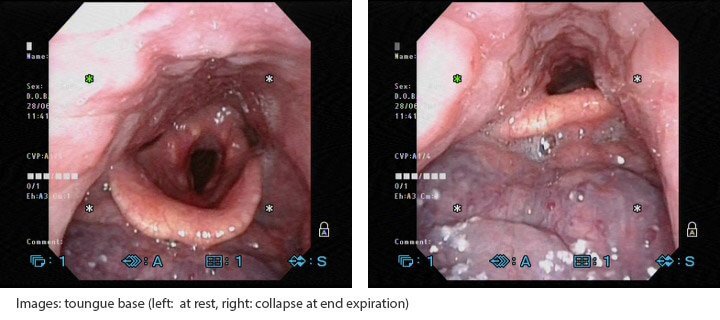
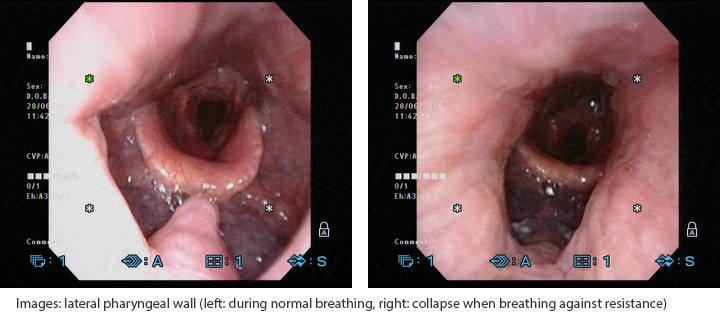
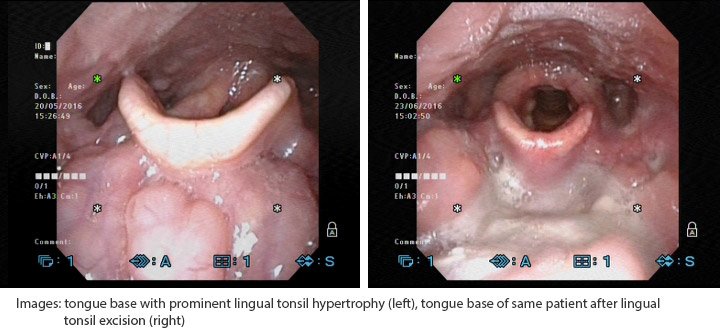
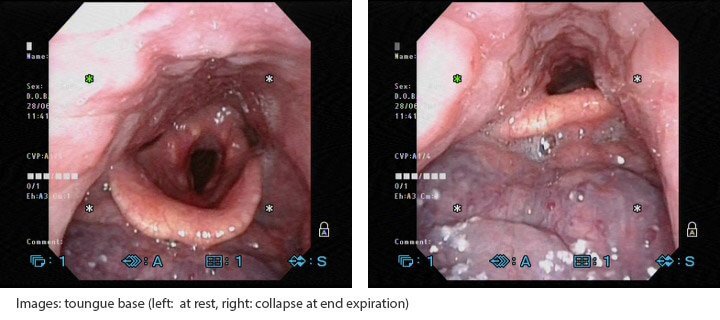
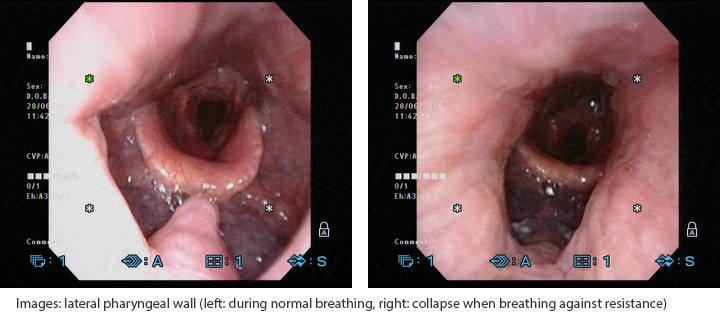
The snoring doctor will examine you with a flexible nasendoscope to determine where the sites of obstruction are.
This helps the snoring specialist decide if surgery is necessary, and if so, to predict the surgical success
rate.
- Nose
- Adenoid Tissue (back of the nose)
- Soft Palate
- Tonsils
- Lateral Pharyngeal Walls (side of throat)
- Tongue Base
- Epiglottis
Treatments for Obstructive Sleep Apnea
- Sleep Hygiene
- May be sufficient snoring treatment for those with mild OSA
- It may include:
- Lying on one’s side
- Propping one’s back up with a wedge pillow while sleeping
- Avoiding alcohol and cigarettes before bedtime
- Get regular and sufficient sleep
- Weight Loss
- Fat deposited within the tongue, muscles and soft tissues of the upper airway and neck increases the risk of them collapsing during sleep
- Weight loss and its maintenance is a key component in the management of OSA
- Mandibular Advancement Appliance (MAD)
- The MAD advances the lower jaw and its contents (tongue) and increases the tension in the muscles that keep the upper airway open during sleep
- Only eligible for some patients who snore or who have mild to moderate OSA
- Continuous Positive Airway Pressure (CPAP) Device
- A device that is worn at night during sleep
- The patient wears a mask over his nose (and or mouth) which is connected to the CPAP machine
- Air is blown into the mask which splints the upper airway open with a column of air
-
CPAP has the best snoring treatment outcomes in the management of OSA and is recommended for the majority of patients

- However, it is also associated with poorer long-term compliance rates due to its inconvenience and some discomfort
- Surgery
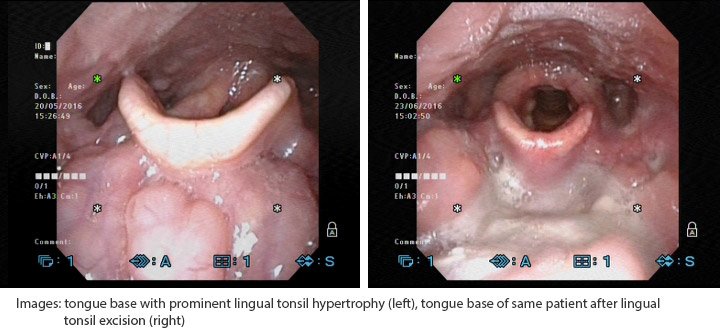
- Very individualised; it can be performed on:
- The nasal cavity (to reduce nasal obstruction)
- The throat (to reduce laxity and increase the dimensions of the upper airway)
- The tongue (to reduce volume and also to advance the tongue)
-
Not all are suitable for surgery
- Upper Airway Stimulation (UAS) System
- A hypoglossal nerve stimulation system implanted beneath the skin to relieve upper airway obstruction during sleep for uninterrupted rest.
- Two incisions are made: in the upper right chest where the small hypoglossal nerve stimulator device is placed; and just under the chin where the hypoglossal nerve is located.
- The device consists of a small battery and two small wires, and is controlled with a small, handheld remote for turning on before bed and off in the morning, or pausing during the night if needed.
- This therapy is suitable for moderate to severe Obstructive Sleep Apnea adult patients with an apnea-hypopnea index (AHI) between 15 and 65, who do not benefit from CPAP treatment.
- It is not intended for patients with a complete concentric collapse at the level of the soft palate, or those in whom central and mixed apneas make up 25% or more of their apnea-hypopnea index.
FAQs About Snoring
How do I know if I have obstructive sleep apnea?
Snoring can signal obstructive sleep apnea if:
- It is loud enough to disturb others
- You wake up gasping or choking
- Your bed partner notices pauses in your breathing during sleep
- You experience excessive daytime drowsiness
Can sleep apnea go away on its own?
No, sleep apnea does not go away on its own. Lifestyle changes and medical treatments like CPAP or surgery are often needed to manage symptoms and prevent complications.
Is snoring & obstructive sleep apnoea (OSA) serious?
Snoring is usually harmless. However, snoring linked to OSA is a serious condition that can lead to:
- Cardiovascular problems (hypertension, arrhythmias, heart attack, heart failure)
- Type 2 diabetes
- Stroke
- Liver problems
What is the best sleeping position for OSA?
Sleeping on your side is generally recommended for individuals with obstructive sleep apnea (OSA). This position
helps keep the airway open by preventing the tongue and soft tissues from collapsing backward.
Helpful Links
-
Read Dr Mok's research paper on Tongue Base Obstruction in OSA: Click Here
-
Read Dr Mok's This Quarterly article on sleep apnea: Click Here
-
Watch Dr Mok’s video about understanding and managing OSA: Click Here